Find trends in your claims documents at scale
Quickly identify patterns across multiple claims with AI-powered cross-case analysis. Detect trends, compare key data points, and surface insights to make more informed decisions—all in one seamless platform
A control center for claims intelligence
Detect patterns across claims, from provider inconsistencies to recurring treatments, helping you act before risks escalate.


Extract key details from past claims to identify trends, improve decision-making, and optimize case strategy.
Extract key data from past claims to compare cases and make faster, informed decisions.


Every claim you process in Wisedocs is reviewed by our team of medical experts to ensure no key details are missed.
.png)
.png)
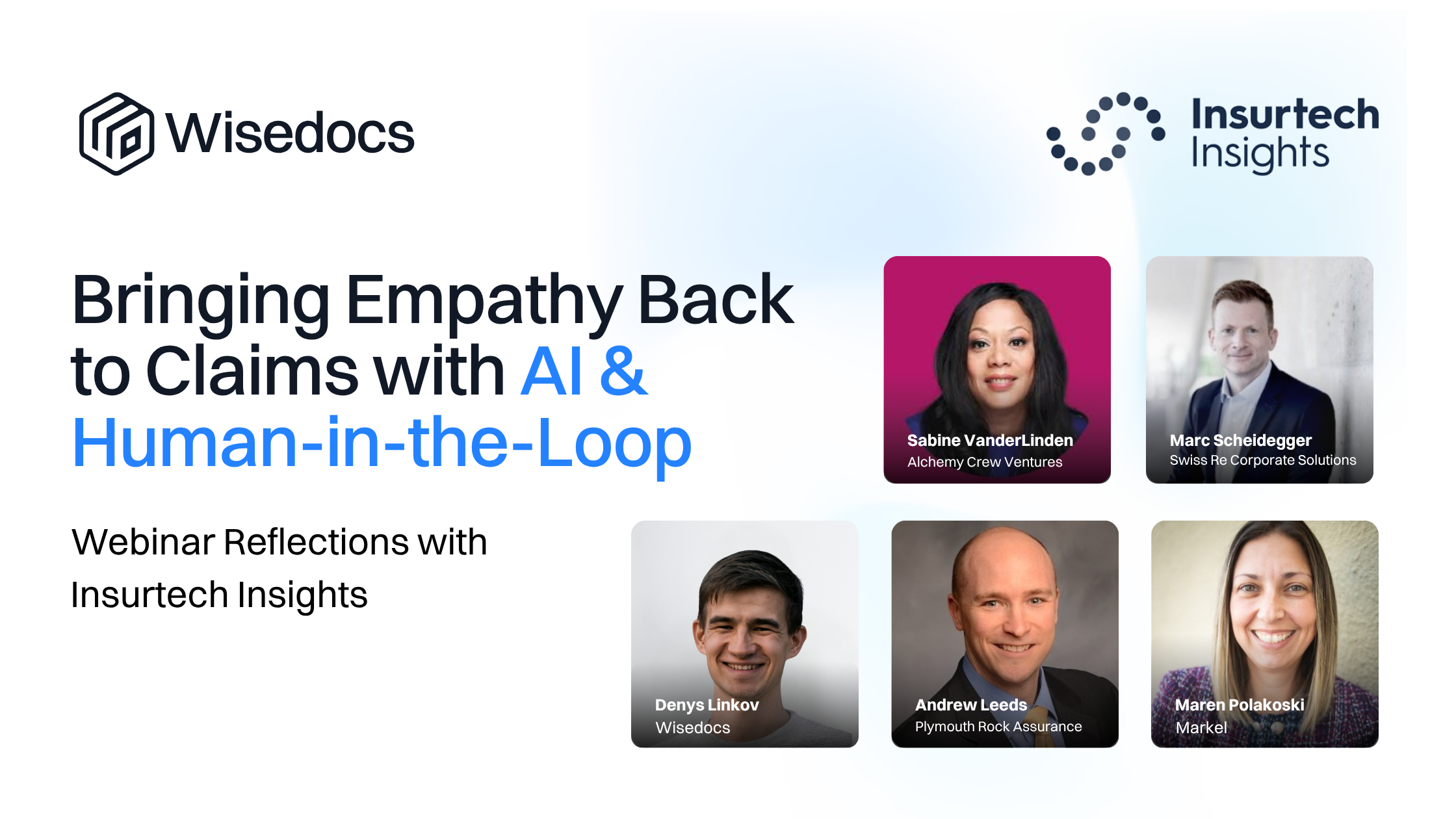
Why Wisedocs
Streamline medical chronology reviews without missing key details and worrying about compliance.


Custom, automated summaries
Generate AI-powered summaries tailored to case needs, with human experts refining key medical insights for legal and insurance use.

Instant document deduplication
Wisedocs flags incorrect claimant information and removes duplicate records instantly.

Claims-specific AI, along with expert human oversight
Wisedocs’ AI is trained on over 60M claims documents, every claims review thats processed is then reviewed by our team of medical experts to validate the information a...

Advanced search & indexing. Find key information in minutes
Locate key medical events instantly with hyperlinked, searchable records, enhanced by human quality checks for context.
Compare claims with organization-wide insights
Identify patterns, detect inconsistencies, and flag potential fraud across multiple claim cases.

Organization-wide claims comparison
Claims teams can compare open and closed cases across the organization, identifying trends in claim resolutions.

Identify risks and inconsistencies
AI flags patterns of fraud, inconsistencies in claims, and repetitive trends, helping teams refine their approach.

Automate 30/60/90-day claim reviews
Adjusters and claims leaders can automate periodic reports to track case status, streamlining compliance and oversight.

Data-backed decision-making
With historical and real-time insights, stakeholders can optimize claims handling, ensuring defensible and efficient resolutions.
Insights & announcements
Strategic updates, expert perspectives, and product highlights from Wisedocs.

.png)