Supporting every stakeholder in workers’ compensation claims resolution
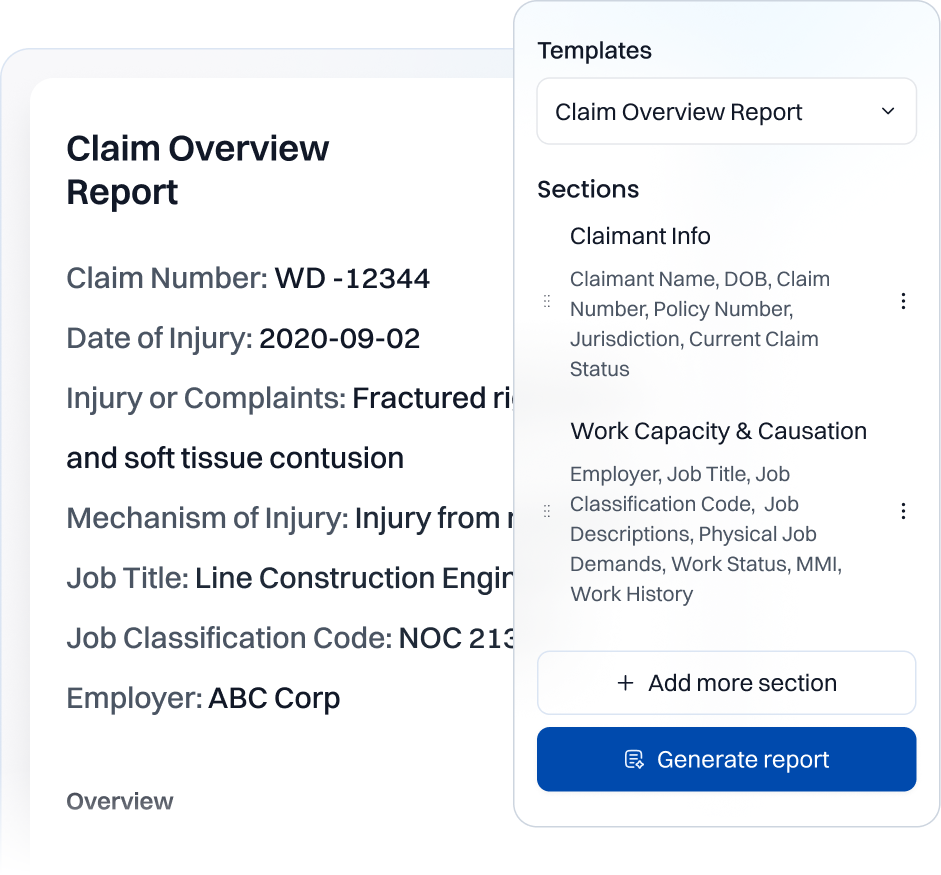
Workers’ compensation claims demand speed, accuracy, and cost efficiency. With Wisedocs, carriers, legal teams, and medical experts specializing in workers’ comp claims can streamline claim document review and accelerate decision-making — all while maintaining accuracy and compliance.







.png)
.png)
.avif)
.avif)
.avif)
.avif)
.avif)



.png)


