The Enterprise Playbook for Human-Powered Claims
Wisedocs’ recently released guide “Rebuilding Trust in AI: Using Human-Assisted Intelligence for Enterprise Claims Transformation”, reveals why the insurance industry lags in AI adoption and how forward-thinking carriers can gain a competitive advantage through human-assisted intelligence. Let’s take a look at some highlights from the guide.
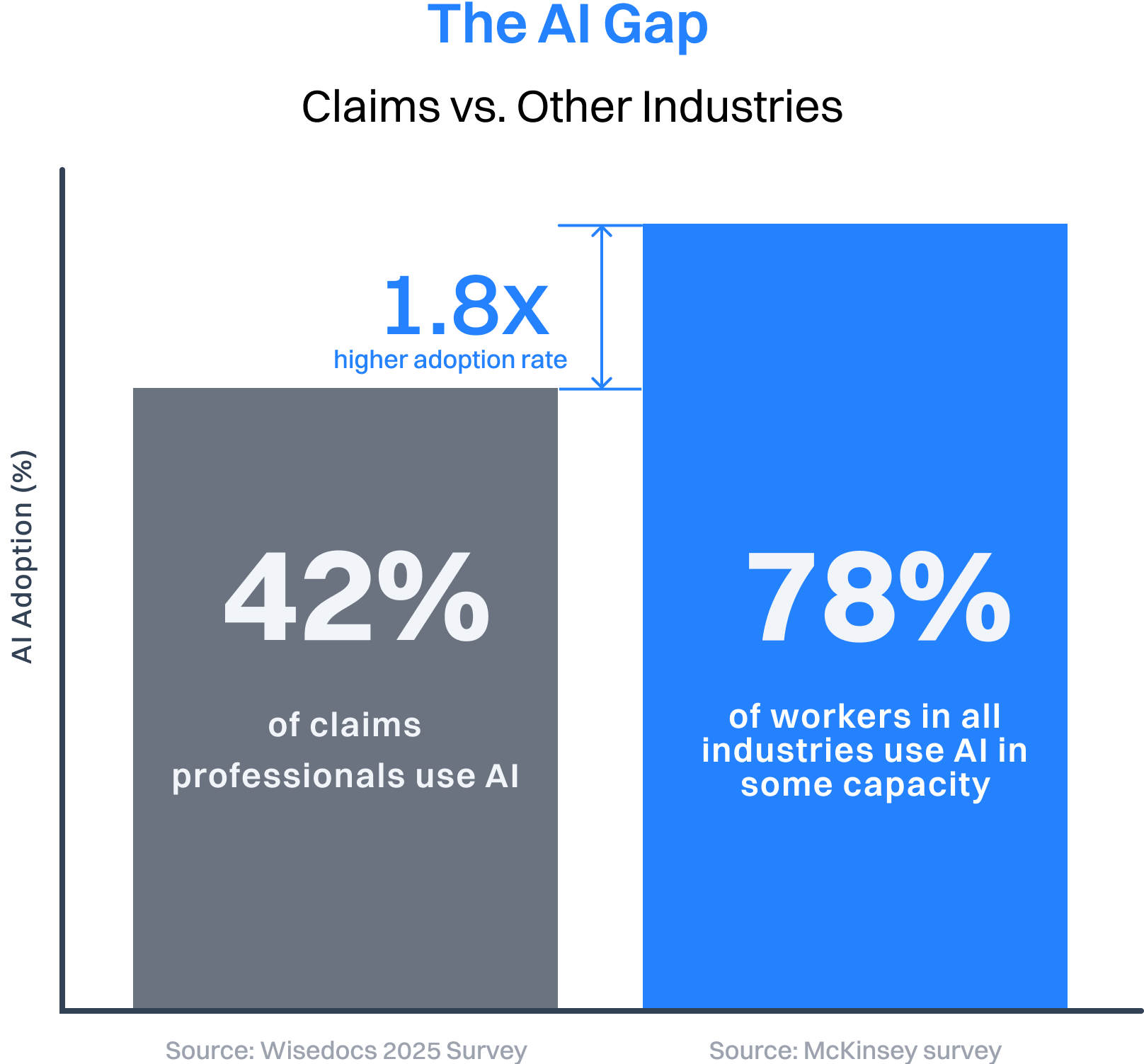
The insurance industry is currently facing a paradox: while 78% of workers across all industries use AI in some capacity, only 42% of claims professionals have embraced this technology. This 1.8x adoption gap isn’t just a statistic; it represents a massive competitive opportunity for forward-thinking enterprises. In Wisedocs’ recently released guide “Rebuilding Trust in AI: Using Human-Assisted Intelligence for Enterprise Claims Transformation”, it reveals why the insurance industry lags in AI adoption and how forward-thinking carriers can gain a competitive advantage through human-assisted intelligence. Let’s take a look at some highlights from the guide.
The AI Fatigue Factor
Many insurance carriers have already attempted autonomous AI solutions that promised instant processing and dramatic cost savings. The reality? These tools fell short on accuracy, leaving enterprises disappointed and hesitant to try again. This AI fatigue has created an industry-wide reluctance to embrace new technology, even as other sectors surge ahead.
The problem wasn’t with AI itself – it was with the approach.
Why Enterprise Claims Face Unique Challenges
Enterprise carriers operate in a fundamentally different environment than smaller organizations. They manage dozens of product lines across multiple jurisdictions, each with specific regulatory requirements. These widely distributed operations mean coordinating scattered document storage, numerous tools, and multiple offices, creating exponentially complex workflows.
Add to this the looming talent shortage, where 22% of claims adjusters are expected to retire before 2026, and the reality that plaintiffs are now using AI to find friendly jurisdictions and profile insurance companies’ legal approaches. The stakes have never been higher.
The Limits of Generalized AI
According to Gartner, Intelligent Document Processing (IDP) solutions are designed to automate the ingestion, processing, and integration of documents across systems.
But Gartner issues a critical caveat:
“No single IDP vendor can process every type of document and its content without optimization, and most align to particular sets of document types or industries.”
Medical and legal documentation make up the bulk of every claim file — and in such high-stakes industries, they can’t be left to generic, fully autonomous AI for case review and resolution. Out of this need for compliance, accuracy, and defensibility, a new category has emerged: the Claims Documentation Platform (CDP). Purpose-built for insurance, CDPs are trained on industry data and regulations, delivering the domain-specific partnership enterprises can trust.
.png)
This crucial step of industry-trained solutions was often overlooked by enterprises, overshadowed by the gleam of promised cost savings and instant processing times. The result: underestimated document complexity, gaps in regulatory compliance, and failed change management. Ultimately, these missteps left enterprise carriers and claims organizations with broken promises — and a clear need for a more practical, defensible path forward.
Even the new generation of industry-specific claims documentation platforms has often failed to deliver what the claims industry truly needs — because they overlooked the critical role of human-in-the-loop oversight. Without expert validation, even the most advanced AI falls short on accuracy, compliance, and defensibility.
The Human-in-the-Loop Breakthrough
Today’s approach for innovative claims processing isn’t fully autonomous AI; it’s human-assisted intelligence. This design combines domain-specific AI models trained on claims documents with expert human oversight, delivering what Wisedocs’ research calls “the 4x trust multiplier.”
In the 2025 survey report “AI in claims and the 4x trust effect of human oversight”, only 16% of claims professionals expressed medium or high trust in AI-generated outputs alone. When expert validation was added, trust jumped to nearly 60% – a 4x increase. This isn’t just about moving faster; it’s about moving correctly with accuracy, traceability, and defensibility at every step.
Human-Powered CDPs: The Strategic Move Forward
When Wisedocs asked claims professionals which part of their process they most want AI to improve, 69% identified document automation and data extraction as the most impactful area. This makes perfect sense – every claim starts and ends with documentation.
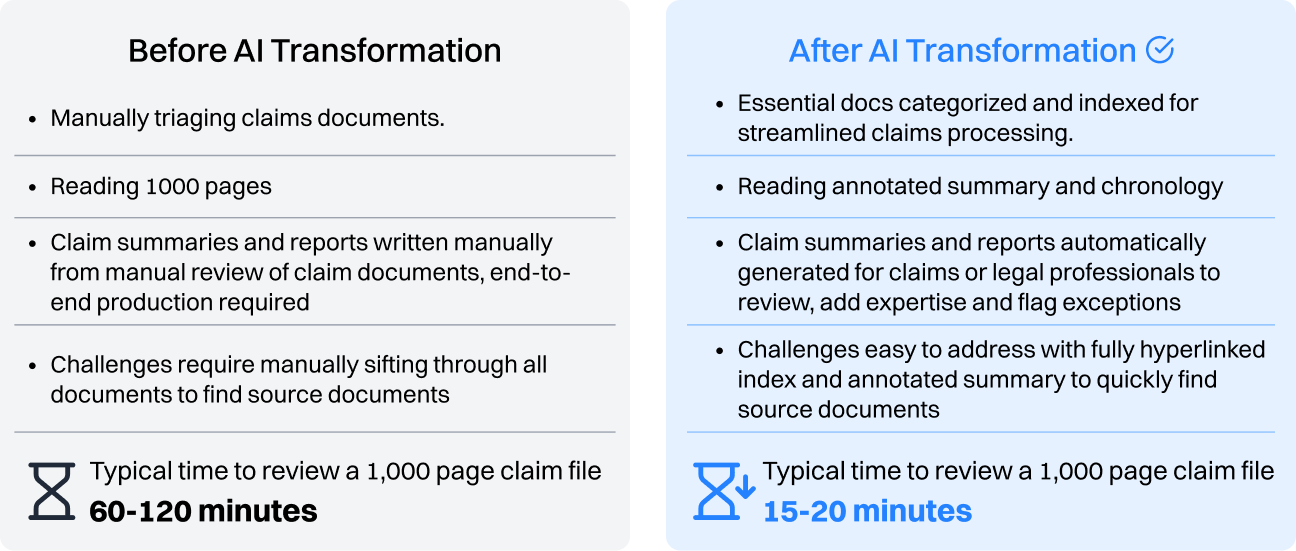
Consider the math: manually reviewing a 1,000 page claim file can take as much as 3-4 hours. Modern Claims Documentation Platforms (CDPs) can reduce this same task to 15-20 minutes of AI-processed summaries with human validation – an 80% reduction that allows adjusters to focus on investigation and customer service rather than document review.
The Enterprise Implementation Playbook
Successful enterprise transformations follow a clear pattern. They start small with a single workflow at one location, focusing on the most labor-intensive and repetitive tasks first. Wisedocs’ five-phrase approach for scaling AI-powered documentation found in the Enterprise Claims Guide ensures smooth implementation while effectively managing change.
The results speak for themselves. One regional state carrier achieved a 60% reduction in document turnaround time, $100K+ in cost savings within the first month, and $1.2M in projected annual savings.

Your Enterprise Claims Transformation Starts Now
We’re in the blue sky phase of AI claims transformation. While 75% of claims professionals believe AI can improve efficiency, 58% aren’t using it yet. This gap represents a strategic advantage for enterprises ready to act.
Wisedocs is committed to being your partner in the next step of claims transformation. In the guide we outline the most common pitfalls enterprises face — and how to avoid them. From the risks of building vs. buying to the dangers of overlooking regulatory requirements, this playbook is designed to help you start strong. Trusted by leading insurance carriers, state funds, and government agencies, Wisedocs brings proven expertise to every stage of your transformation.
Industry innovation doesn’t wait for everyone. The carriers implementing human-in-the-loop AI today will set the standard for tomorrow’s claims processing, while others struggle to catch up.
Ready to explore how Claims Documentation Platforms can improve your enterprise operations? Download the complete Enterprise Claims Transformation Guide today.


.png)


